ACLS Protocol
ACLS Certification
This comprehensive guide covers everything you need to know about ACLS protocol and the critical role it plays in equipping healthcare providers with vital life-saving skills for treating cardiac emergencies. Sign up for eMedCert’s ACLS courses now to stay up-to-date with the latest ACLS guidelines and techniques!

The Efficient, Affordable Way to Certify
The eMedCert Online ACLS (Advanced Cardiac Life Support) Certification course is built specifically for the demanding lifestyle required of 21st-century healthcare professionals and students. Our 100% online course gives you control of your ACLS Certification – take it when you want, where you want, and at your own pace. Complete your course with efficiency from your desktop, tablet, or smartphone.
Credible and Affordable ACLS Certification
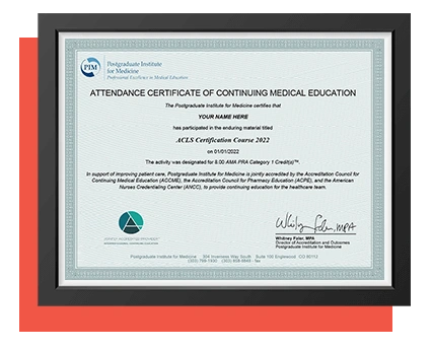
Our Advanced Cardiac Life Support (ACLS) training is accredited through our partnership with the Postgraduate Institute for Medicine (PIM) and also by the California Board of Registered Nursing (CA BRN). We provide AMA, ANCC, ACPE, and ADA continuing education credits, redeemable upon completion of the ACLS Certification course.
eMedCert and our ACLS materials undergo routine audits by regulatory organizations and 3rd-party clinical teams. Our internal medical team continuously works to ensure compliance, accuracy, and integrity.
Ready To Begin?
Complete your registration and begin reviewing your material in less than two minutes. Certification has never been this easy!
Online ACLS Certification Details
Our ACLS Certification course is designed to deliver the best online certification experience that can accompany your busy schedule.
- Start When Ready -- No Time Limit -- Available 24/7
- Finish in a Single Sitting or Save Your Progress and Return Later
- Achieve a Passing Score –– 80% or Higher (40 Correct / 50 Total Questions)
- Instant Exam Results & Unlimited Exam Retakes
- No On-Site Skills Check Required
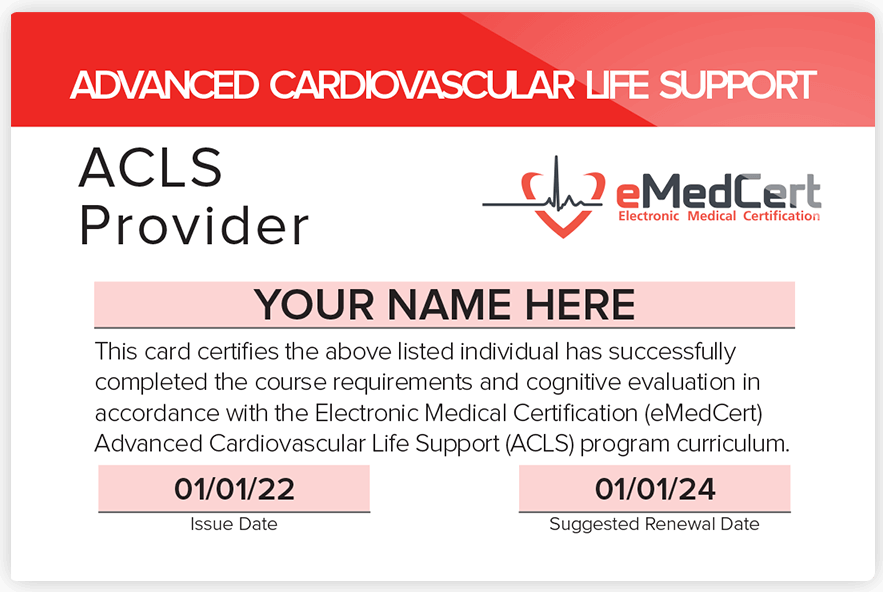
- Digital ACLS Provider Card Available Immediately for Download
- 8.0 AMA, ANCC, ACPE or ADA CME Credits Available
Trusted By:




ACLS Protocol
Following ACLS protocol is pivotal in improving patient outcomes in emergency medical care. ACLS resuscitation procedures are a lifeline for healthcare providers in the most challenging circumstances, specifically during cardiac arrest. But what exactly is ACLS, and why is it so crucial in healthcare?
What Is ACLS Protocol?
Advanced Cardiac Life Support (ACLS) is a set of standardized procedures designed to swiftly and effectively address life-threatening situations. It covers everything from recognizing signs of cardiac arrest to delivering prompt, evidence-based interventions at a time when every second counts. To get ACLS certified, providers must take an ACLS certification course, followed by an ACLS recertification course every 2 years.
The Significance of ACLS Protocol for Cardiac Arrest:
Cardiac arrest is a critical situation where the heart suddenly stops beating effectively. It often results in loss of consciousness, and the affected person may become disabled or die if not treated immediately.
In such dire moments, the ACLS protocol becomes the script healthcare providers follow to deliver high-quality cardiopulmonary resuscitation (CPR) and administer crucial medications that can potentially revive a patient's failing heart. It provides a systematic approach, ensuring that health professionals swiftly and accurately assess and treat the patient.
The significance of ACLS resuscitation becomes apparent when we consider that cardiac arrest can happen anywhere, at any time, and to anyone. It is not limited to hospital settings; it can occur in homes, workplaces, and public spaces. This is why the protocol is adaptable to different environments and provider levels.
Whether you're a nurse, physician, physician's assistant, EMT, anesthesiologist, dentist, or specialist, ACLS training equips you with the skills and knowledge needed to respond effectively. Essentially, ACLS is the roadmap that guides medical professionals through high-stress situations involving cardiac emergencies.
Related: Who Needs ACLS Training?
ACLS Protocols for Nurses
Nurses are often at the forefront of patient care, and ACLS certification for nurses enhances their ability to respond competently to critical situations. It provides nurses with a structured framework to address a variety of medical emergencies, including strokes, cardiac crises, and conditions necessitating CPR intervention.
Let's explore how ACLS protocols empower nurses to make a difference in critical moments.
Stroke Management
One crucial area of focus in ACLS training for nurses is stroke management. Time is of the essence when it comes to this medical emergency, as rapid intervention can significantly improve a patient's chances of recovery.
ACLS-trained nurses are well-versed in recognizing the signs and symptoms of strokes, such as facial drooping, slurred speech, and limb weakness. They're ready to quickly initiate the necessary interventions and deliver the correct medications, imaging, and assessments as per the ACLS stroke protocol. The goal of ACLS training for stroke management is clear: minimize the damage caused by the stroke and improve the patient's outcome.
Moreover, ACLS-trained nurses are skilled in emotionally supporting stroke patients and their families. They understand the anxiety and fear accompanying a stroke diagnosis and can offer reassurance and guidance, creating a compassionate, comforting environment.
CPR Protocol in ACLS
CPR is the immediate response to maintain oxygenation and circulation in emergencies where a patient's heart has stopped beating effectively. It's a skill that every nurse should possess.
The ACLS course covers CPR techniques that prioritize high-quality compressions and proper ventilation. Nurses learn the correct compression depth, rate, hand placement, and ventilation strategies so each compression maximizes blood flow to the vital organs.
Nurses trained in ACLS can perform CPR in multiple situations, including sudden cardiac arrest, pulseless ventricular tachycardia, and ventricular fibrillation.
Handling Cardiac Emergencies
ACLS gives nurses the tools to respond to any ACLS cardiac emergency. Nurses certified in ACLS are proficient in the use of defibrillators, medications like epinephrine, and advanced airway management techniques. This ensures they act decisively and skillfully, even in flat-line protocol ACLS scenarios.
ACLS Case Scenarios: Realistic Training for Nurses
ACLS training goes beyond theory. Nurses undergo training that simulates real-world emergencies to practice their skills in a more realistic setting. This firsthand approach ensures nurses are well-prepared to act confidently when the moment arrives.
ACLS Interventions
ACLS interventions encompass a wide range of procedures, protocols, and pharmacological approaches that enable health professionals to respond effectively to many complex medical situations. They equip healthcare workers with the skills to resuscitate and stabilize patients facing life-threatening conditions.
These interventions are grounded in the latest medical guidelines. They are continually updated to reflect advancements in the field to ensure that ACLS-certified professionals are equipped with current knowledge and techniques.
Key components of ACLS interventions include:
- CPR: ACLS-certified professionals are trained to deliver high-quality CPR. This is vital for maintaining blood circulation and oxygen delivery during cardiac episodes.
- Defibrillation: ACLS procedure involves the use of defibrillators to deliver electric shocks to restore a normal heart rhythm when necessary.
- Medication administration: ACLS-accredited individuals understand using medications like epinephrine, amiodarone, and vasopressors to correct abnormal rhythms and stabilize patients.
- Advanced airway management: This involves skills in techniques such as endotracheal intubation and supraglottic airway placement to secure and maintain a patient's airway.
- Cardiac monitoring: ACLS-certified professionals must be able to interpret cardiac rhythms on monitors, identify arrhythmias, and make rapid treatment decisions.
Here is how an online ACLS course equips you to respond effectively to complex medical emergencies:
Adequate Training
An ACLS certificate indicates that the holder has undergone specialized training in cardiac life support management. The coursework covers a wide range of critical interventions, including advanced airway management, defibrillation, cardiac monitoring, and medication administration. This equips health professionals with the knowledge and skills to confidently assess and manage life-threatening situations.
Systematic Approach
ACLS certification emphasizes a systematic approach to patient care. Healthcare providers are trained to prioritize actions based on the patient's condition, ensuring immediate life-threatening issues are addressed first. The ACLS interventions sequence enhances the chances of a positive outcome.
Pharmacological Expertise
ACLS-certified professionals have a solid understanding of medications used in resuscitation efforts, including indications, dosages, and potential side effects of ACLS drugs. This knowledge is critical in administering medications like epinephrine, amiodarone, and atropine, which are tailored to specific cardiac rhythms and clinical applications.
Adaptability
ACLS training online teaches adaptability. Healthcare providers can adjust interventions based on the patient's response and evolving conditions, thus optimizing patient-centric care in high-stress situations.
Confidence and Competence
An ACLS class imparts knowledge and fosters the confidence and competence needed in high-stress medical emergencies. Healthcare providers with ACLS certification are prepared to make rapid, informed decisions, enhancing patient outcomes.
ACLS Steps
ACLS protocol outlines the actions to take in scenarios requiring the delivery of CPR protocols. Here are some of the important ACLS steps for unresponsive patients:
Assess the Situation
The first step in ACLS is to assess the patient and scene. Ensure both you and the patient are safe and free from harm. Then, check if the patient is responsive and breathing by gently tapping and shouting to check for any response.
Activate Emergency Response
If the patient is unresponsive and not breathing or breathing is abnormal, activate the emergency response system or call for help immediately.
Airway Management
Ensure the patient's airway is clear and open. Use techniques like the head-tilt-chin-lift or jaw-thrust maneuver to achieve this. Look, listen, and feel for chest rise and fall. If the patient isn't breathing or is breathing abnormally, initiate rescue breathing.
Try to maintain adequate oxygenation and ventilation. You can use a bag-mask device to support the patient's breathing.
Check for a Pulse
Assess for a pulse within 10 seconds. If there's no pulse or a pulse below 60 beats per minute, initiate CPR.
Start High-Quality CPR
Begin high-quality CPR by pushing hard and fast in the center of the chest. Deliver CPR according to ACLS protocol at a rate of 100-120 compressions per minute, at a depth of at least 2 inches for adults.
Ensure a full chest recoil between compressions and minimize interruptions. If you use a bag-mask device with high-flow oxygen, maintain a compression-to-ventilation ratio of 30:2.
Rhythm Analysis
If available, attach an AED or heart monitor to keep track of the patient's cardiac rhythm. If a shockable rhythm (ventricular fibrillation or pulseless ventricular tachycardia) is detected, deliver a shock following the AED prompts for defibrillation.
Administer Medications
Administer medications based on specific cardiac rhythm, ACLS guidelines, and clinical scenarios. Ensure proper dosages and routes of administration.
Continuous CPR
Immediately after medication administration or defibrillation, resume high-quality CPR. Reassess the patient's rhythm and pulse. Continue monitoring the patient's cardiac rhythm; if it remains shockable, repeat defibrillation as necessary. If not shockable, provide appropriate interventions based on the rhythm.
Post-Cardiac Arrest Care
When the return of spontaneous circulation (ROSC) is achieved, focus on post-cardiac arrest care, which includes optimizing ventilation, oxygenation, and blood pressure to treat the underlying cause of the arrest. Monitor the patient's vital signs, cardiac rhythm, and response to interventions and adjust treatment strategies accordingly.
Documentation
Maintain accurate and timely documentation of all interventions, medications administered, and the patient's response for comprehensive medical records.
Throughout the process, adhere to ACLS algorithms. These are updated regularly and reflect the latest research and best practices. Observe these guidelines to deliver appropriate interventions.
Remember that effective communication and teamwork are crucial in ACLS scenarios. Assign specific roles to team members, ensure clear communication, and switch compressors regularly to prevent fatigue.